Impaired pressure is a significant factor in obesity research, affecting both physical and mental health. We will explore the implications of impaired pressure and its impact on weight gain and overall well-being.
Understanding the interplay between pressure and obesity can provide valuable insights into effective prevention and treatment strategies. It is crucial to address this issue as an integral part of holistic health management. By identifying the underlying mechanisms and developing interventions to mitigate impaired pressure, we can make substantial progress in combatting the obesity epidemic.
In the following sections, we will delve deeper into the scientific research surrounding impaired pressure, its effects on the body, and potential interventions to promote healthier lifestyles.

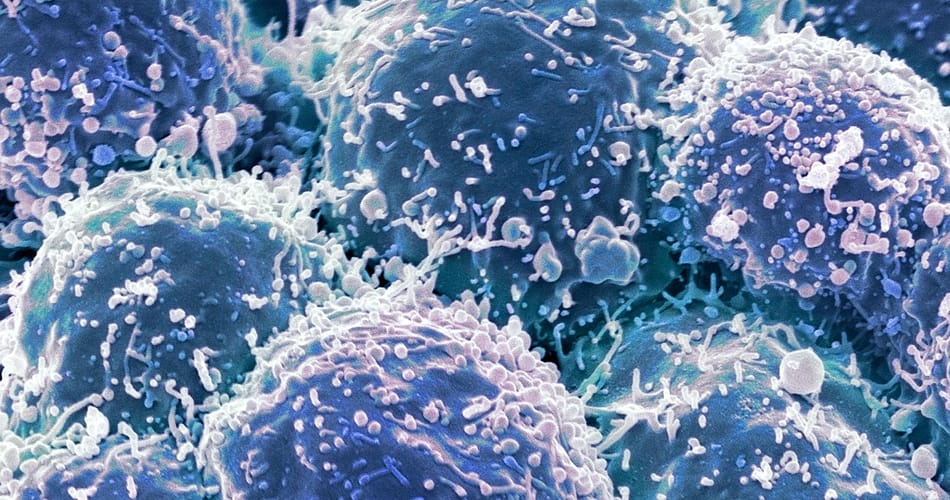
Credit: www.umc.edu
Understanding The Link Between Obesity And Hypertension
This Obesity Research article sheds light on the impaired pressure observed in individuals suffering from obesity and hypertension. The link between these two conditions is explored in-depth, providing valuable insights into their interconnected nature.
Prevalence Of Obesity And Hypertension
Obesity and hypertension, or high blood pressure, are two of the most prevalent health issues worldwide. They often go hand in hand, with obesity increasing the risk of developing hypertension. Here are some key points to understand the link between obesity and hypertension:
- Obesity affects approximately 13% of the global population, leading to various health complications, including hypertension.
- Hypertension, also known as the “silent killer,” affects about 30% of adults, making it a major public health concern.
- The prevalence of both obesity and hypertension is increasing at an alarming rate, posing a significant burden on healthcare systems.
Exploring The Relationship Between Body Weight And Blood Pressure
The relationship between body weight and blood pressure is complex and multifaceted. Here are some essential insights:
- Excess body weight, particularly excess adipose tissue, increases the workload on the heart, leading to elevated blood pressure.
- The accumulation of visceral fat, located around the abdominal organs, is strongly associated with hypertension.
- Research shows that weight loss, even as little as 5-10% of body weight, can significantly decrease blood pressure levels.
- Other factors, such as insulin resistance, inflammation, and hormonal imbalances, further contribute to the obesity-hypertension link.
Understanding the mechanisms behind obesity-related hypertension is crucial for developing effective prevention and treatment strategies. By addressing obesity and promoting a healthy lifestyle, we can reduce the burden of hypertension and improve overall cardiovascular health.
Mechanisms Behind Obesity-Induced Hypertension
The article in Obesity Research highlights the impaired pressure mechanisms responsible for obesity-induced hypertension. It delves into the link between obesity and high blood pressure, shedding light on the underlying physiological processes.
Role Of Insulin Resistance And Inflammation:
- Insulin resistance, a condition where cells become less responsive to the effects of insulin, plays a significant role in obesity-induced hypertension.
- When insulin resistance occurs, the body produces more insulin, which may lead to increased sodium retention and elevated blood pressure.
- Inflammation, another mechanism behind obesity-induced hypertension, can occur as a result of excess adipose tissue. Inflammatory markers such as CRP and cytokines can contribute to high blood pressure.
Impact Of Adipose Tissue On Blood Pressure Regulation:
- Adipose tissue, commonly known as fat, secretes various molecules known as adipokines that can influence blood pressure regulation.
- Adipokines such as resistin, visfatin, and adiponectin have been found to impact blood pressure through various mechanisms, including vascular inflammation and endothelial dysfunction.
- Excessive accumulation of adipose tissue can lead to increased adipokine production, contributing to the development of hypertension.
Influence Of Leptin And Adipokines On Hypertension Development:
- Leptin, a hormone secreted by fat cells, is involved in regulating appetite and energy expenditure. However, in obesity, leptin levels become elevated, leading to a condition known as leptin resistance.
- Leptin resistance disrupts the normal signaling pathways involved in blood pressure regulation, potentially contributing to hypertension.
- Adipokines, including leptin, can also influence the sympathetic nervous system, leading to increased sympathetic activity and higher blood pressure.
Insulin resistance and inflammation play important roles in obesity-induced hypertension. Additionally, adipose tissue and its secreted molecules, such as adipokines and leptin, influence blood pressure regulation. By understanding these mechanisms, researchers aim to develop strategies to prevent and manage hypertension in individuals with obesity.
Effects Of Uncontrolled Hypertension On Organ Systems
Uncontrolled hypertension can have significant effects on various organ systems, as discussed in an article in Obesity Research. The impairment in blood pressure regulation can lead to complications in the cardiovascular, renal, and neurological systems, highlighting the importance of managing hypertension effectively.
Damage To The Heart And Blood Vessels
Uncontrolled hypertension can have detrimental effects on the heart and blood vessels, leading to serious health complications. Here are some potential damages related to this condition:
- Increased workload on the heart: High blood pressure puts extra strain on the heart by forcing it to pump harder to circulate blood throughout the body.
- Coronary artery disease: Uncontrolled hypertension can cause the arteries supplying blood to the heart to narrow and harden, leading to coronary artery disease.
- Heart failure: The heart’s constant effort to overcome the elevated blood pressure can weaken it over time, eventually resulting in heart failure.
- Stroke: Hypertension can damage blood vessels in the brain, making them more susceptible to blockages or ruptures which can lead to a stroke.
- Aneurysm formation: High blood pressure weakens the walls of blood vessels, increasing the risk of aneurysm development. A ruptured aneurysm can be life-threatening.
Renal Complications And Kidney Disease
Uncontrolled hypertension can have detrimental effects on the kidneys, potentially leading to various renal complications and kidney disease. A few potential implications include:
- Chronic kidney disease (CKD): Hypertension is a leading cause of CKD, as elevated blood pressure damages the small blood vessels in the kidneys, reducing their ability to function properly.
- Kidney failure: If left uncontrolled, hypertension can progress to kidney failure, where the kidneys lose their ability to filter waste products and excess fluid from the body.
- Albuminuria: High blood pressure can result in the presence of proteins, such as albumin, in the urine. This condition, known as albuminuria, is an early sign of kidney damage.
- Renal artery stenosis: Hypertension can contribute to the narrowing of the renal arteries, reducing blood flow to the kidneys and potentially causing damage.
Neurological And Cognitive Implications
Uncontrolled hypertension can also negatively impact the brain and cognitive function. Some potential implications include:
- Cognitive decline: Chronic hypertension is associated with an increased risk of cognitive decline and dementia. The reduced blood flow to the brain can affect cognitive abilities such as memory, attention, and problem-solving.
- Transient ischemic attacks (TIAs): Uncontrolled hypertension can lead to TIAs, often referred to as “mini-strokes,” which occur due to temporary disruptions in blood flow to the brain. These episodes can cause temporary neurological issues.
- Vascular dementia: Hypertension damages blood vessels in the brain, increasing the risk of vascular dementia, a condition resulting from reduced blood supply to the brain.
- Increased risk of stroke: Hypertension is a significant risk factor for stroke, and uncontrolled high blood pressure can further increase this risk. A stroke can lead to various neurological impairments, depending on the affected brain region.
Remember, controlling hypertension through lifestyle modifications and appropriate medical interventions is crucial to mitigate these potential damages to organ systems.
Secondary Complications Of Hypertension In Obesity
The article in obesity research explores the secondary complications arising from hypertension in individuals with obesity. It delves into the impaired pressure regulation system in this context.
Obesity and hypertension often go hand in hand, leading to a host of secondary complications. In this section, we will explore some of these complications, shedding light on the effects obesity has on our bodies. From metabolic syndrome and insulin resistance to the increased risk of cardiovascular disease, as well as the association with sleep apnea and respiratory disorders, let’s delve into the details.
Metabolic Syndrome And Insulin Resistance:
- People with obesity often develop metabolic syndrome, which is a cluster of conditions such as high blood sugar, high blood pressure, and abnormal cholesterol levels.
- Insulin resistance is a common occurrence in obesity, where the body’s cells fail to respond properly to insulin, leading to elevated blood sugar levels.
Increased Risk Of Cardiovascular Disease:
- Obesity places significant strain on the cardiovascular system, increasing the risk of conditions like heart disease, stroke, and heart failure.
- Excess weight causes the heart to work harder to pump blood, leading to hypertension and the deposition of fatty plaques in the arteries.
Association With Sleep Apnea And Respiratory Disorders:
- Obese individuals are more likely to experience sleep apnea, a condition characterized by interrupted breathing during sleep.
- Sleep apnea can lead to excessive daytime sleepiness, fatigue, and an increased risk of developing respiratory disorders such as chronic obstructive pulmonary disease (COPD).
These secondary complications highlight the profound impact obesity can have on our overall health. It is crucial to address obesity and manage hypertension effectively to mitigate the risk of these complications. Whether through lifestyle changes or medical interventions, taking steps to combat obesity is essential for our well-being.
Lifestyle Modifications For Blood Pressure Control
Lifestyle changes can effectively control blood pressure levels, according to an obesity research article. These modifications can include a healthier diet, regular exercise, stress management, and avoiding tobacco and alcohol.
Importance Of A Balanced Diet And Weight Management
Maintaining a balanced diet and managing weight play a crucial role in controlling blood pressure. By making the right food choices and achieving a healthy weight, individuals can significantly lower their risk of developing high blood pressure or improve existing conditions.
Here are some lifestyle modifications that can help in blood pressure control:
- Consuming a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats is vital for overall health. A diet that is low in sodium, saturated fats, and added sugars can specifically assist in managing blood pressure.
- Limiting sodium intake to less than 2,300 milligrams per day (and even lower for individuals with hypertension) can effectively lower blood pressure. Reducing the consumption of processed foods, canned goods, and restaurant meals known for their high sodium content is recommended.
- Following the Dietary Approaches to Stop Hypertension (DASH) eating plan, which emphasizes low sodium and high potassium intake, has been proven to help lower blood pressure.
- Watching portion sizes and practicing mindful eating can aid in weight management. Overeating can lead to weight gain, increasing the risk of high blood pressure.
- Achieving and maintaining a healthy weight can have a significant impact on blood pressure control. Losing as little as 5-10% of body weight can result in lower blood pressure levels.
Regular physical activity should also be incorporated into the lifestyle modifications for blood pressure control.
Medical Interventions For Hypertension Management
Medical interventions for hypertension management are crucial in addressing impaired pressure. This article in Obesity Research highlights effective strategies to overcome hypertension, providing valuable insights for managing this condition.
Hypertension, also known as high blood pressure, can have serious health implications if left uncontrolled. Fortunately, there are various medical interventions available to manage hypertension effectively. These interventions range from medications commonly prescribed for hypertension treatment to bariatric surgery as a potential option for blood pressure control.
Medications Commonly Prescribed For Hypertension Treatment:
- Angiotensin-Converting Enzyme (ACE) Inhibitors: These medications help relax blood vessels, making it easier for the heart to pump blood.
- Angiotensin II Receptor Blockers (ARBs): ARBs block the effects of angiotensin II, a hormone that causes blood vessels to narrow.
- Calcium Channel Blockers (CCBs): CCBs prevent calcium from entering the muscles of the heart and blood vessels, leading to a relaxation of these muscles and lowering blood pressure.
- Diuretics: Diuretics help your body eliminate excess sodium and water, reducing the volume of blood flowing through your blood vessels.
- Beta-Blockers: These medications reduce the workload on the heart, making it easier for the heart to pump blood effectively.
These medications are typically prescribed based on factors such as the severity of hypertension, the presence of any underlying medical conditions, and the patient’s individual needs.
Bariatric Surgery As A Potential Option For Blood Pressure Control:
Bariatric surgery, commonly used for weight loss purposes, has shown promising results in managing hypertension in some individuals. Here are a few key points to consider regarding bariatric surgery as a potential option for blood pressure control:
- Weight Reduction: Bariatric surgery helps individuals achieve significant weight loss, which often leads to a reduction in blood pressure levels.
- Metabolic Changes: The surgical procedures involved in bariatric surgery can lead to metabolic changes that positively impact blood pressure regulation.
- Improvement in Obesity-Related Conditions: Bariatric surgery can improve or resolve various obesity-related conditions, such as diabetes and sleep apnea, which can contribute to hypertension.
It’s important to note that bariatric surgery is generally considered a last resort for individuals who have not achieved adequate blood pressure control through lifestyle modifications and medications. Additionally, the decision to undergo bariatric surgery should be made in consultation with a healthcare professional experienced in managing hypertension and obesity.
Medical interventions play a crucial role in effectively managing hypertension. With a range of medications available and bariatric surgery as a potential option, individuals can work with healthcare professionals to find the most suitable approach for their specific needs. Prioritizing blood pressure control through medical interventions can significantly improve overall health outcomes for individuals with hypertension.
Holistic Approaches To Blood Pressure Reduction
Explore innovative holistic approaches to effectively lower blood pressure in a groundbreaking obesity research article. Discover evidence-based strategies that prioritize a comprehensive and natural wellness approach to managing blood pressure impairment.
The management of blood pressure extends far beyond medication, as there are several holistic approaches that can effectively reduce hypertension. By incorporating stress management and relaxation techniques, as well as complementary therapies into daily routines, individuals can make significant strides in maintaining healthy blood pressure levels.
Let’s explore these holistic approaches in detail.
Stress Management And Relaxation Techniques:
- Deep breathing exercises: Engaging in deep breathing exercises, such as diaphragmatic breathing, can promote relaxation and help lower blood pressure.
- Meditation: Practicing meditation for a few minutes each day can reduce stress, anxiety, and subsequently, blood pressure levels.
- Yoga: The combination of gentle movements, controlled breathing, and meditation in yoga can have a positive impact on blood pressure.
- Tai chi: This ancient Chinese practice involves slow, deliberate movements and deep breathing, which can help in stress reduction and blood pressure management.
- Progressive muscle relaxation: By systematically tensing and relaxing different muscle groups, progressive muscle relaxation can alleviate muscle tension and promote relaxation, leading to lower blood pressure.
Complementary Therapies And Their Impact On Hypertension:
- Acupuncture: Stimulating specific acupoints through the insertion of thin needles can assist in blood pressure regulation.
- Herbal remedies: Certain herbs, such as garlic, hawthorn, and basil, have been traditionally used to support cardiovascular health and may aid in blood pressure reduction.
- Massage therapy: Regular massage sessions can help relax the body and reduce stress, which can contribute to lower blood pressure.
- Aromatherapy: The use of essential oils, like lavender and chamomile, through inhalation or diluted application, can have calming effects and potentially lower blood pressure.
- Mind-body techniques: Practices like biofeedback, guided imagery, and mindfulness-based stress reduction can be beneficial in managing hypertension.
By embracing these holistic approaches and incorporating them into daily routines, individuals can make positive strides in reducing blood pressure levels, leading to improved overall health and well-being. Remember, a holistic approach encompasses not only physical health but also mental and emotional well-being, making it a comprehensive and effective method for blood pressure reduction.
Public Health Initiatives And Education Campaigns
Obesity Research introduces an article on impaired pressure, focusing on public health initiatives and education campaigns. The study sheds light on the importance of effective strategies in addressing obesity and promoting healthier lifestyles.
Policies Aimed At Promoting Healthy Lifestyles
- Implementing policies that promote healthy lifestyles is a crucial step in combating obesity and its associated health risks.
- Here are some key points to consider:
- Encouraging healthy food options: Implementing regulations that promote the availability and affordability of nutritious foods in public places such as schools, workplaces, and recreational areas can help individuals make healthier diet choices.
- Restricting marketing of unhealthy products: Policies that limit the advertising and marketing of high-calorie, low-nutrient foods and beverages can reduce the exposure and influence of such products on individuals, particularly children.
- Creating supportive environments: Developing policies that encourage physical activity by improving access to safe parks, recreational facilities, and active transportation options can help people incorporate regular exercise into their daily routine.
- Incorporating health education in schools: Introducing comprehensive health education programs in schools can equip students with essential knowledge and skills to make informed decisions about nutrition, physical activity, and overall well-being.
- Collaborating with food industries: Engaging food manufacturers, distributors, and retailers in initiatives that promote healthier products, reformulate existing ones, and provide clear nutritional labeling can contribute towards creating a healthier food environment.
Importance Of Community Education And Awareness Programs
- Community education and awareness programs play a crucial role in addressing obesity by empowering individuals and communities to make healthier choices.
- Consider the following points:
- Spreading knowledge about healthy habits: Community education programs can provide information on the importance of balanced nutrition, portion control, regular physical activity, and the risks associated with obesity. This knowledge equips individuals with the tools they need to make healthier lifestyle choices.
- Targeting vulnerable populations: Education programs that specifically focus on vulnerable populations, such as low-income communities or ethnic minorities, can help reduce health disparities by addressing the unique challenges they face. These programs can provide culturally sensitive resources and support networks to promote healthy behaviors.
- Collaboration with healthcare professionals: Partnerships between community organizations and healthcare professionals can enhance the effectiveness of education campaigns. By involving physicians, nurses, and dietitians, these initiatives can provide evidence-based information and personalized guidance to individuals seeking to improve their health.
- Engaging community leaders: Building strong relationships with local leaders, such as religious figures, community organizers, and influential individuals, can amplify the reach of education programs. By involving trusted individuals, these initiatives can gain credibility and encourage community-wide participation.
- Utilizing digital platforms: Leveraging digital platforms, including social media, websites, and mobile applications, can widen the reach of education and awareness programs. These mediums allow for targeted messaging, interactive resources, and the sharing of success stories, ultimately motivating individuals to maintain healthier lifestyles.
By implementing policies that promote healthy lifestyles and conducting community education and awareness programs, individuals and communities can work together to combat obesity and improve public health.
Early Detection And Screening Measures
This article in Obesity Research explores the importance of early detection and screening measures in addressing impaired pressure. It discusses the significance of proactive measures in identifying and managing obesity-related health issues.
Obesity is a growing concern around the world, with serious health consequences such as hypertension. Early detection and screening measures play a crucial role in identifying individuals at risk and implementing intervention strategies. In this section, we will explore two key approaches to early detection and screening: regular blood pressure monitoring and evaluating obesity markers for potential hypertension risk.
Let’s delve into each of these measures in more detail.
Regular Blood Pressure Monitoring:
- Regular blood pressure checks are an essential part of early detection and screening for hypertension in individuals who are overweight or obese.
- It involves measuring the force of blood against the walls of the arteries, which can indicate the presence of hypertension.
- Monitoring blood pressure at regular intervals helps healthcare professionals identify high blood pressure early on and develop personalized treatment plans.
- By frequently monitoring blood pressure, healthcare providers can track changes in blood pressure levels and make necessary interventions to prevent complications.
- The procedure is quick, non-invasive, and easily accessible, making it a valuable tool in managing hypertension risk in obese individuals.
Evaluating Obesity Markers For Potential Hypertension Risk:
- Besides blood pressure monitoring, evaluating obesity markers can provide additional insights into an individual’s risk of developing hypertension.
- Body Mass Index (BMI) is a widely used measure to assess obesity and its association with hypertension.
- Obesity-related factors such as waist circumference, waist-to-hip ratio, and body fat percentage can also be evaluated to identify potential hypertension risk.
- Evaluating obesity markers helps healthcare professionals understand the underlying mechanisms linking obesity and hypertension.
- Combining obesity markers with other risk factors such as family history, lifestyle factors, and medical history enables a comprehensive assessment of an individual’s hypertension risk.
Early detection and screening measures are vital in identifying individuals at risk of hypertension due to obesity. Regular blood pressure monitoring and evaluating obesity markers provide valuable insights and enable healthcare professionals to implement timely interventions. By utilizing these measures, healthcare providers can effectively manage hypertension risk in overweight and obese individuals, ultimately improving long-term health outcomes.
Importance Of Multidisciplinary Collaboration In Obesity Research
Multidisciplinary collaboration plays a crucial role in obesity research, enabling experts from different fields to come together and address the complexities of the issue. By combining their knowledge and expertise, researchers can gain a comprehensive understanding of factors contributing to obesity and develop effective interventions for prevention and treatment.
Bridging The Gap Between Healthcare Providers And Researchers
In the field of obesity research, it is crucial to bridge the gap between healthcare providers and researchers. This multidisciplinary collaboration is of paramount importance in order to address the complex and multifaceted nature of obesity and its associated health conditions.
By working together, healthcare providers and researchers can pool their expertise, resources, and knowledge to gain a comprehensive understanding of obesity and develop effective strategies for prevention and treatment. Here are some key points highlighting the significance of this collaboration:
- Holistic approach: Combining the insights and perspectives of healthcare providers and researchers ensures a comprehensive and holistic approach to understanding and tackling obesity. This collaboration allows for a more in-depth analysis of the various factors contributing to obesity, such as genetics, lifestyle, socioeconomic status, and environmental influences.
- Translational research: Collaboration between healthcare providers and researchers facilitates the translation of scientific findings into practical applications. By bridging the gap between theory and practice, this multidisciplinary approach ensures that research outcomes directly benefit patients and the healthcare community as a whole.
- Data collection and analysis: Healthcare providers possess valuable data on patient demographics, medical histories, and treatment outcomes. Researchers can leverage this data to conduct comprehensive studies and analyze the effectiveness of different interventions. This collaboration enhances the quality and validity of research findings, leading to evidence-based recommendations.
- Identifying gaps and challenges: Through collaborative efforts, healthcare providers and researchers can identify gaps in existing research, clinical practices, and healthcare policies related to obesity. By working together, they can develop innovative solutions to address these gaps and overcome the challenges in preventing and managing obesity and its associated health conditions.
- Holistic patient care: Collaborative research allows healthcare providers to gain a deeper understanding of the underlying causes and mechanisms of obesity and its related complications. This knowledge can aid in the development of tailored treatments and interventions, resulting in improved patient outcomes and holistic, patient-centered care.
By fostering collaboration between healthcare providers and researchers, we can unlock new insights, advance our understanding of obesity, and ultimately make significant strides in the prevention and management of this global health issue. Through multidisciplinary collaboration, we can ensure that research findings are translated into practical solutions that directly benefit patients, healthcare providers, and society as a whole.
Frequently Asked Questions For An Article In Obesity Research Impaired Pressure
What Is Obesity Research?
Obesity research is the study of the causes, effects, and treatments of obesity. It aims to understand the complex factors contributing to obesity, including genetics, environment, and lifestyle, in order to develop effective strategies for prevention and management.
How Does Obesity Impair Blood Pressure?
Obesity can impair blood pressure by increasing the workload on the heart and blood vessels. Excess body fat puts pressure on the arteries and leads to the constriction of blood vessels, making it harder for blood to flow freely. This can result in hypertension and other cardiovascular problems.
What Are The Health Risks Associated With Obesity?
Obesity is associated with a range of health risks, including an increased risk of heart disease, type 2 diabetes, high blood pressure, stroke, certain cancers, and respiratory problems. It can also lead to joint pain, sleep apnea, infertility, and psychological issues such as depression and low self-esteem.
How Can Obesity Research Help Prevent And Treat Obesity?
Obesity research plays a crucial role in preventing and treating obesity. By studying the underlying causes, researchers can develop targeted interventions and strategies for weight loss and weight management. This includes identifying effective dietary approaches, lifestyle modifications, and potential pharmaceutical interventions.
Conclusion
The article on obesity research has shed light on the complex connection between impaired pressure and the development of obesity. The findings highlight the importance of understanding the underlying factors that contribute to this relationship. By examining the impact of impaired pressure on fat deposition and metabolism, researchers have made significant strides in unravelling the intricate mechanisms involved in obesity.
This knowledge can potentially pave the way for targeted interventions and treatments, ultimately improving the health outcomes of individuals struggling with obesity. Moreover, the article emphasizes the need for further research to explore the multifaceted aspects of impaired pressure and its implications for obesity.
As we continue to deepen our understanding of this relationship, it is hopeful that more effective strategies for prevention and management of obesity will emerge. Ultimately, this research serves as a stepping stone towards a healthier future for all.